CASE20240522_001
A Challenging Case Report of Transcatheter Aortic Valve Replacement in Bicuspid Aortic Valve in High-Surgical-Risk Patient
By Min Gyu Kang, Han Gyul Kim, Jinsin Koh, jinyong hwang
Presenter
Min Gyu Kang
Authors
Min Gyu Kang1, Han Gyul Kim2, Jinsin Koh1, jinyong hwang1
Affiliation
Gyeongsang National University Hospital, Korea (Republic of)1, SAMSUNG MEDICAL CENTER, Korea (Republic of)2,
View Study Report
CASE20240522_001
TAVR - Bicuspid AV
A Challenging Case Report of Transcatheter Aortic Valve Replacement in Bicuspid Aortic Valve in High-Surgical-Risk Patient
Min Gyu Kang1, Han Gyul Kim2, Jinsin Koh1, jinyong hwang1
Gyeongsang National University Hospital, Korea (Republic of)1, SAMSUNG MEDICAL CENTER, Korea (Republic of)2,
Clinical Information
Relevant Clinical History and Physical Exam
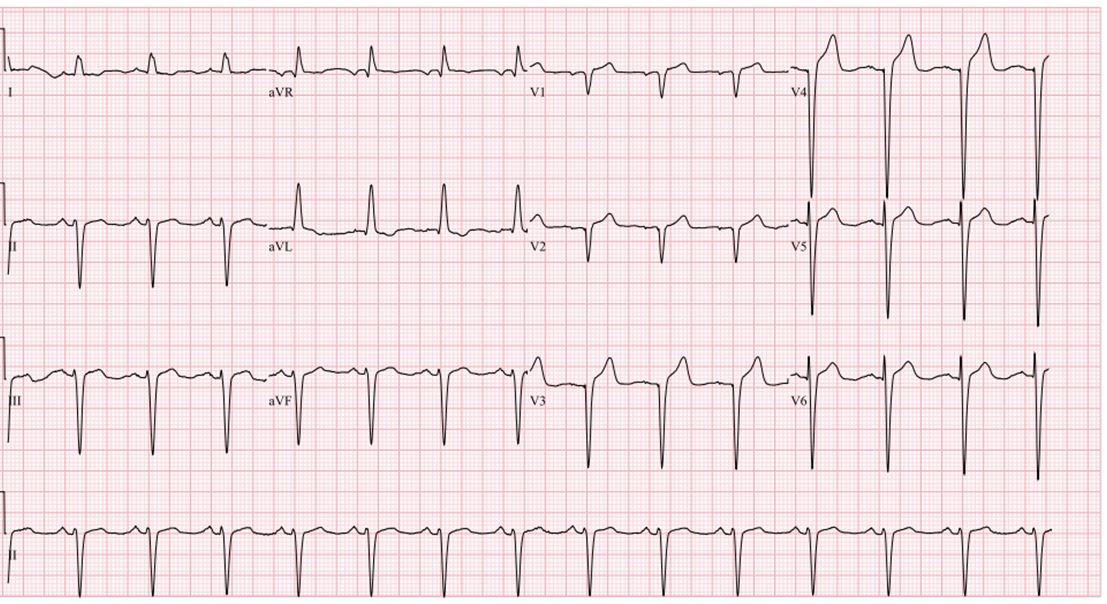
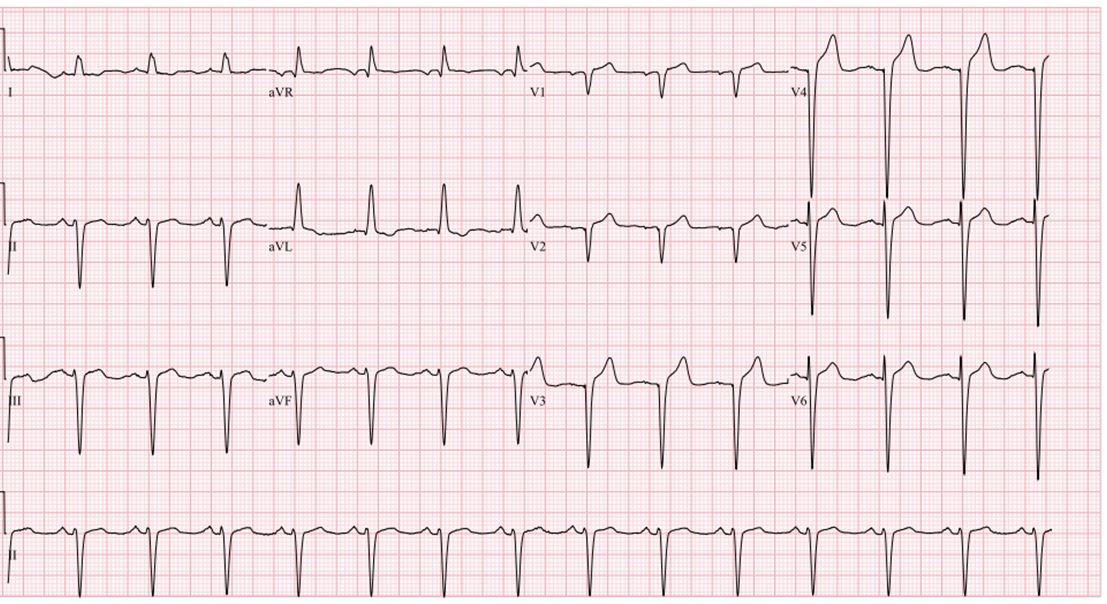
We present the challenging case of a 76-year-old man patient suffering from of dyspnea. He was diagnosed with severe aortic valve regurgitation 20 years ago and was recommended for surgical aortic valve replacement. He had a history of chronic obstructive pulmonary disease requiring home oxygen therapy and was follow-up by medical treatment due to high surgical risk. A systolic heart murmur is auscultated at the right upper sternal border. Electrocardiogram showed a left ventricle hypertrophy.
Relevant Test Results Prior to Catheterization
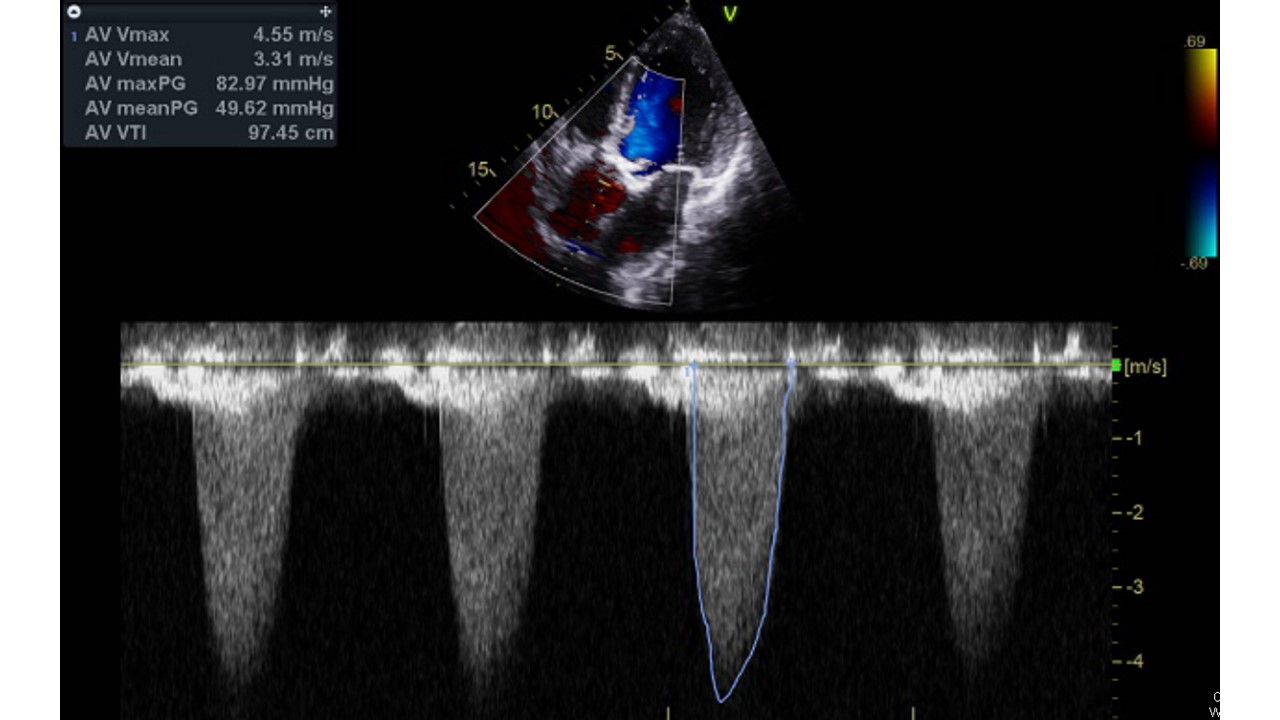
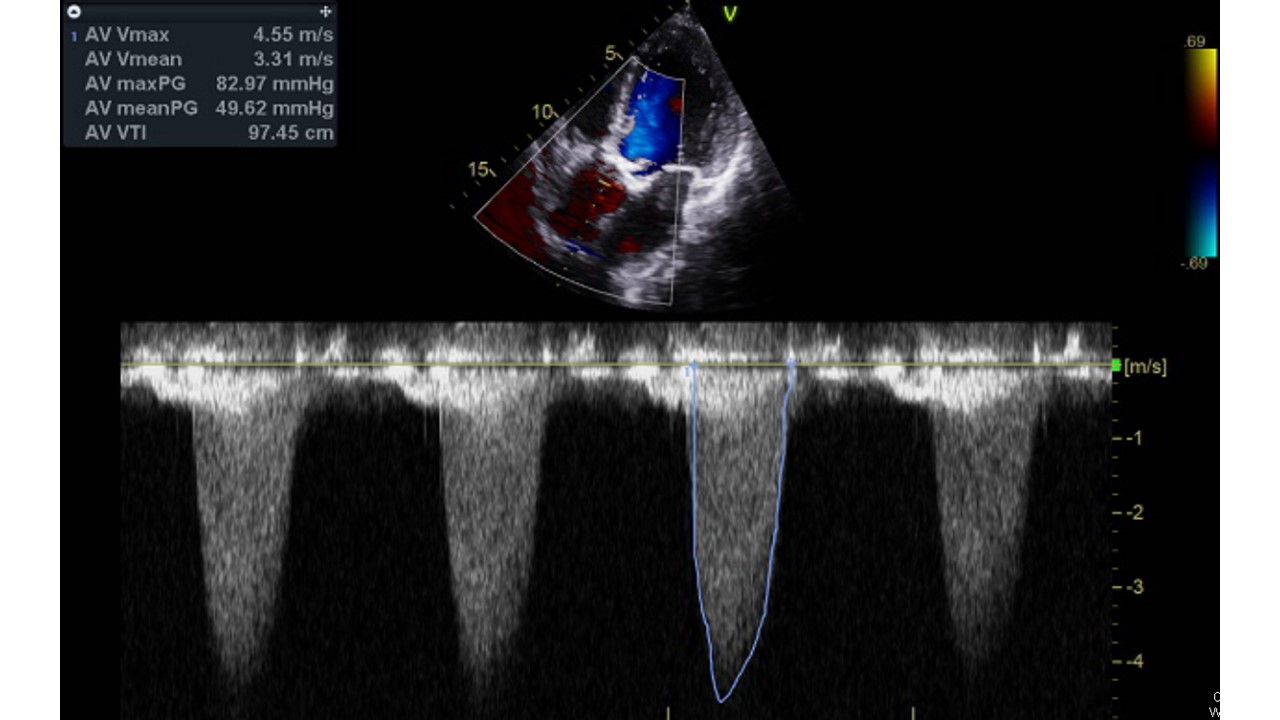
Echocardiography showed findings consistent with severe aortic stenosis (aortic valve Vmax 4.59m/sec, mean pressure gradient 48 mmHg, and aortic valve area 0.74cm2). The aortic valve was a fused bicuspid valve with calcified leaflets. Left ventricle ejection fraction was 28%. Computed tomography showed ascending aorta aneurysm (4.8mm) and bicuspid aortic valve (calcified raphe, Sievers type I). Extended calcification was observed toward the left coronary cusp of the left ventricle out tract.
Relevant Catheterization Findings
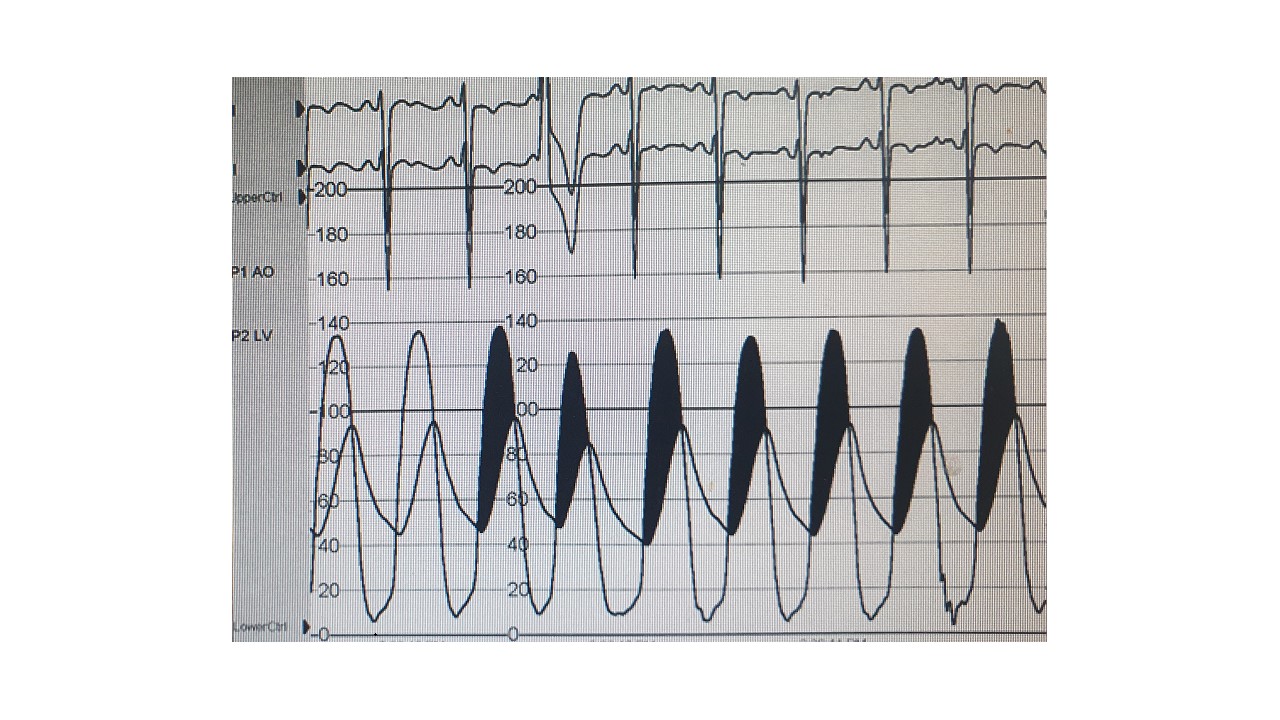
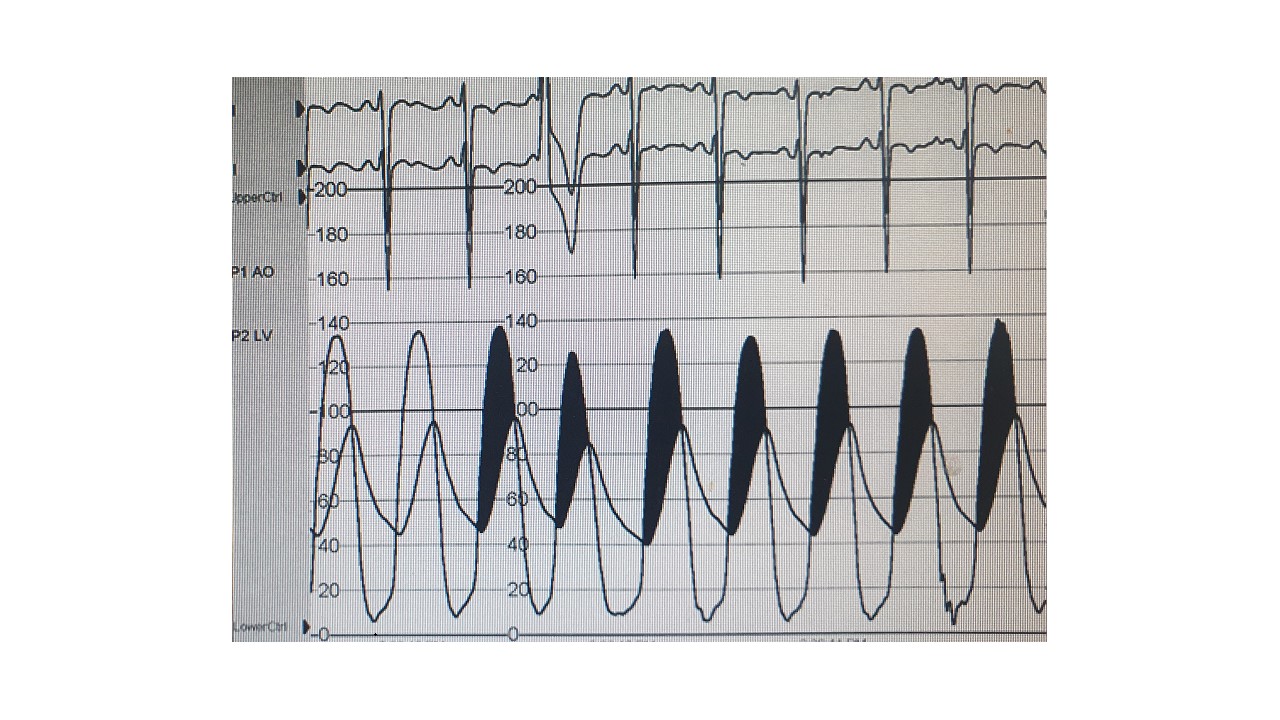
Heart team decided to perform transcatheter aortic valve replacement due to the high risk of surgery (STS score 9.7%, EuroSCORE II 3.62%). Under general anesthesia, vascular access was through the femoral artery. Fluoroscopy showed deep calcification in the direction of the left coronary cusp. No evidence of significant coronary artery stenosis was observed. Simultaneous recording of left ventricular and aortic pressure tracings demonstrated a 45-mmHg mean systolic gradient (shaded area).
 TAVR_1.mp4
TAVR_1.mp4
Interventional Management
Procedural Step
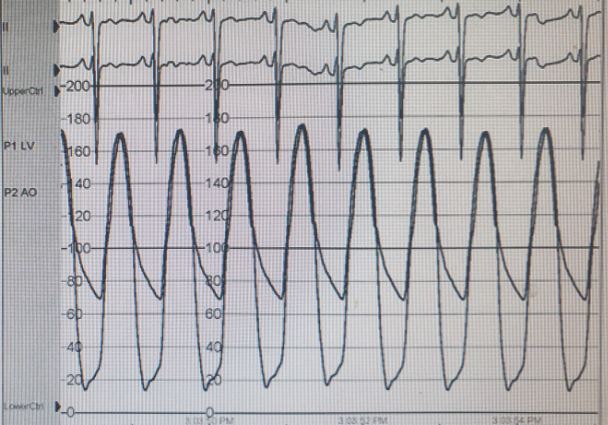
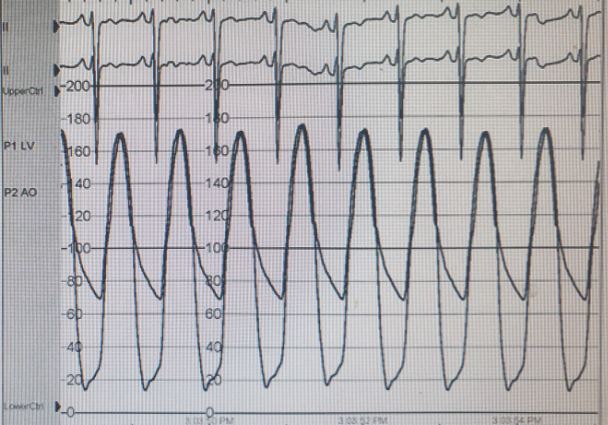
Area derived diameter was 29.7mm (annulus area 693.5mm2) and operator chose a balloon expandable valve (SAPIEN 3 ULTRA 29 mm, Edwards). Balloon valvuloplasty was performed first to overcome the annulus calcification, and a strategy of high implantation with slow inflation was planned for a safer procedure due to extended calcification in the left ventricle out tract. There were no acute complications, including newly appeared aortic regurgitation, after balloon valvuloplasty on transesophageal echocardiography. Under pacing of 180 bpm, prosthetic valve was well positioned even though deep calcification limited full inflation in the left coronary cusp. After prosthetic valve implantation, the patient's vital signs were stable and no significant changes were observed on the electrocardiogram. Transesophageal echocardiography showed little paravalvular leak, and there were no acute complications related to the procedure. Angiography showed no aortic or coronary complications. Simultaneous recording of left ventricular and aortic pressure tracings showed a significant reduction in mean systolic gradient (8-mmHg).
 TAVR_2.mp4
TAVR_2.mp4
 TAVR_3.mp4
TAVR_3.mp4
Case Summary
Our heart team reports a case of transcatheter aortic valve replacement for a bicuspid aortic valve in a patient with high-surgical-risk. This case has a clinical significance in that successful use of balloon expandable valve to treat a patient with high-structural-risk, including bicuspid valve with extended calcification in the left ventricle out tract, and ascending aortic aneurysm, in addition to the patient's clinical risk factors.
