CASE20240520_001
How Small Can the Neo-LVOT Be in Transcatheter Mitral Valve Replacement Using the LAMPOON Procedure
By Huan-Chiu Lin, Yung-Tsai Lee, Tien Ping Tsao, Wei-Hsian Yin
Presenter
Huan-Chiu Lin
Authors
Huan-Chiu Lin1, Yung-Tsai Lee1, Tien Ping Tsao1, Wei-Hsian Yin1
Affiliation
Cheng Hsin General Hospital, Taiwan1,
View Study Report
CASE20240520_001
Mitral Valve Intervention - Transcatheter MV Replacement
How Small Can the Neo-LVOT Be in Transcatheter Mitral Valve Replacement Using the LAMPOON Procedure
Huan-Chiu Lin1, Yung-Tsai Lee1, Tien Ping Tsao1, Wei-Hsian Yin1
Cheng Hsin General Hospital, Taiwan1,
Clinical Information
Relevant Clinical History and Physical Exam
We describe a case of a 67-year-old female with underlying diseases of hypertensive cardiovascular disease, type 2 diabetes mellitus, and chronic kidney disease; ten yearsbefore, she underwent mitral valve repair with surgical annuloplasty ring due to severe mitral regurgitation. She presented to our hospital with functional class III heart failure symptoms. Physical examination revealed grade IV/VI systolic murmur over apex, with bilateral lower limbs pitting edema.
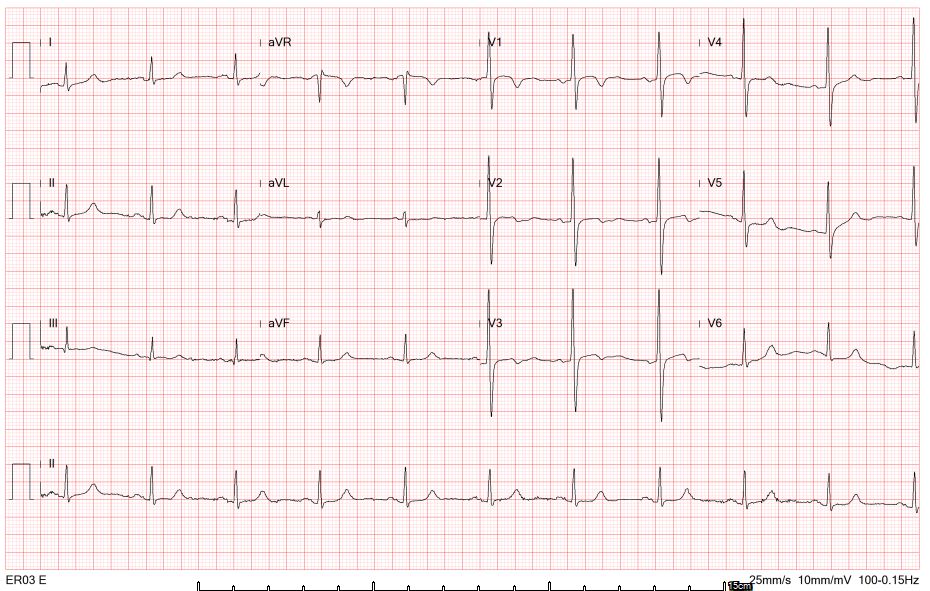
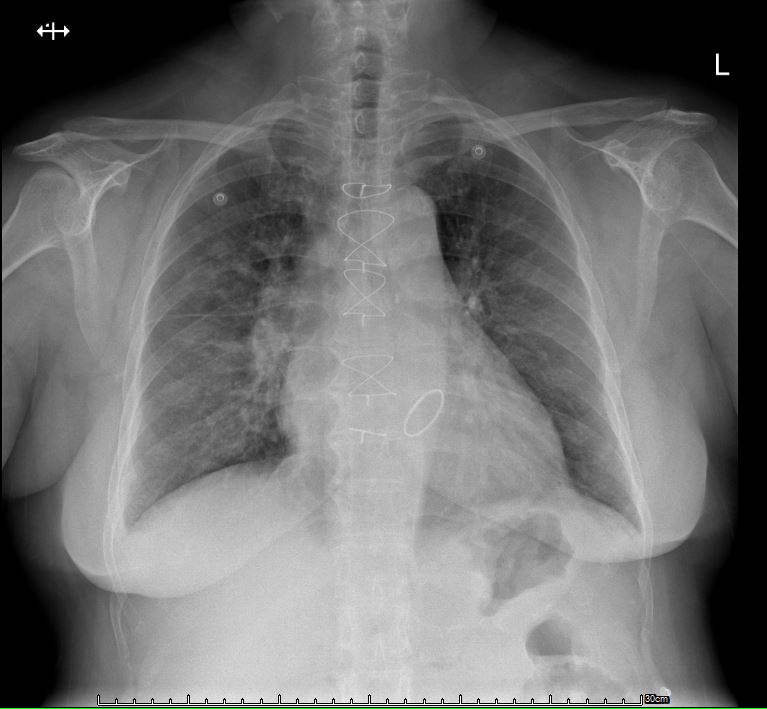
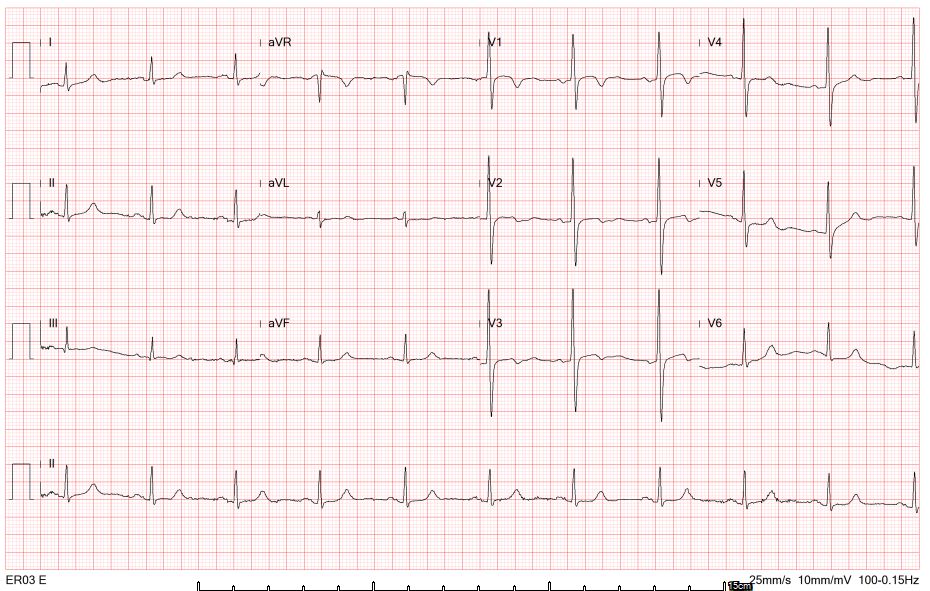
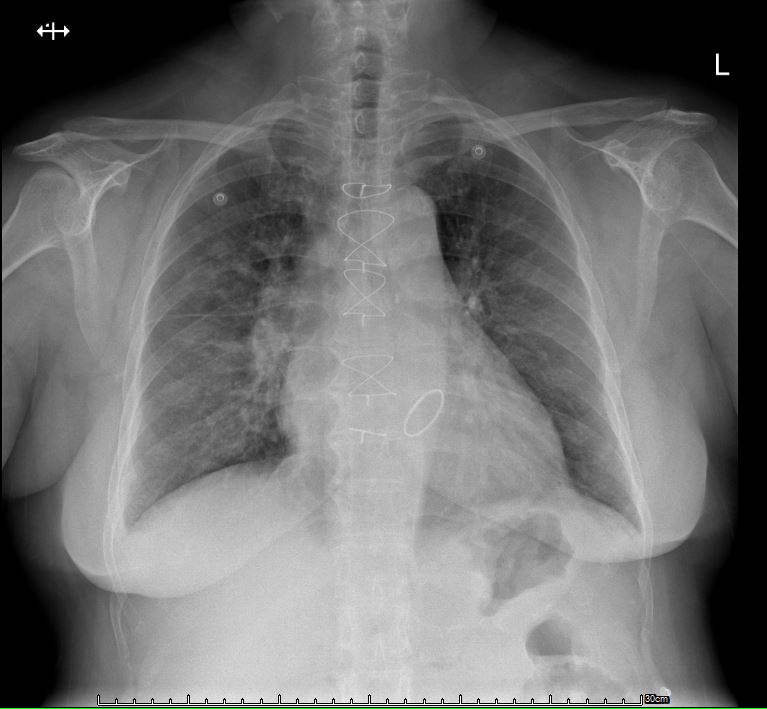
Relevant Test Results Prior to Catheterization
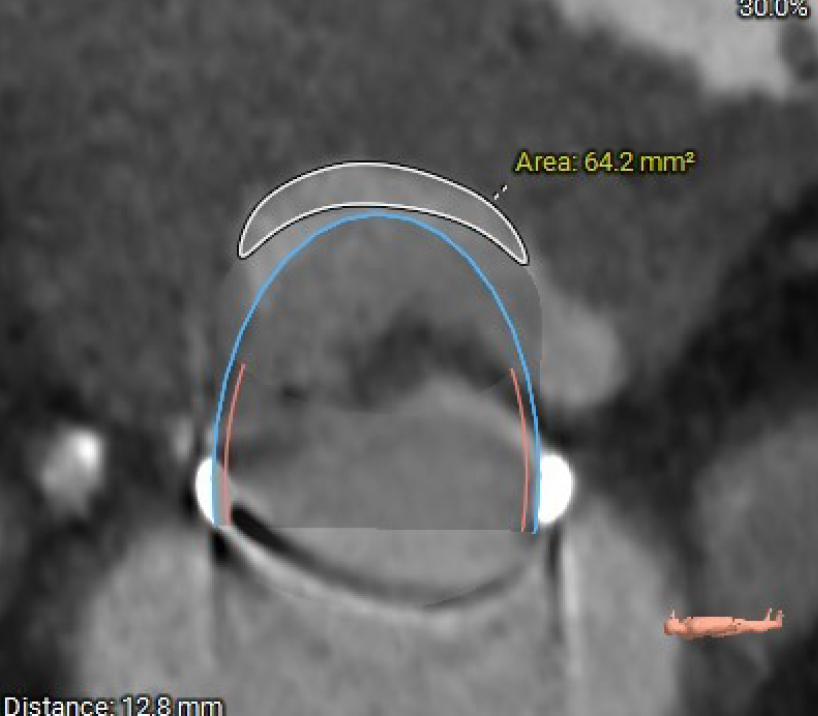
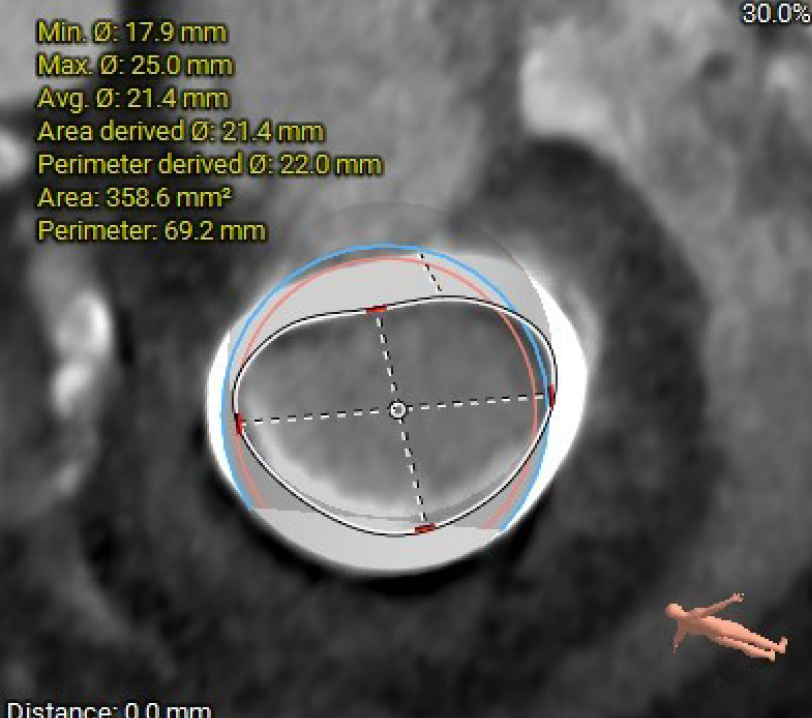
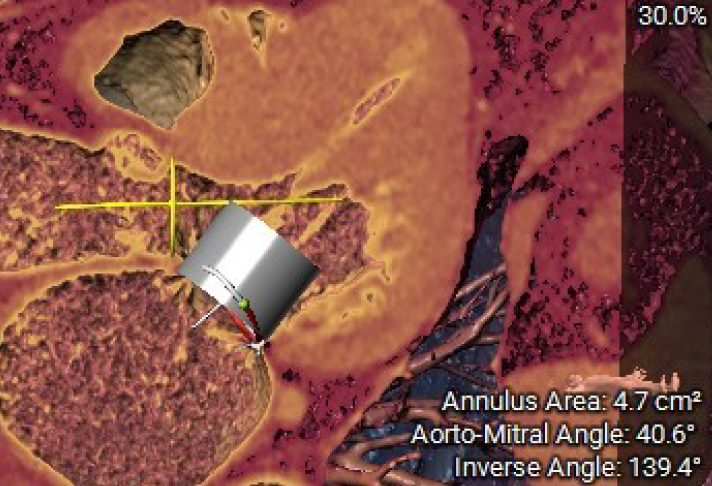
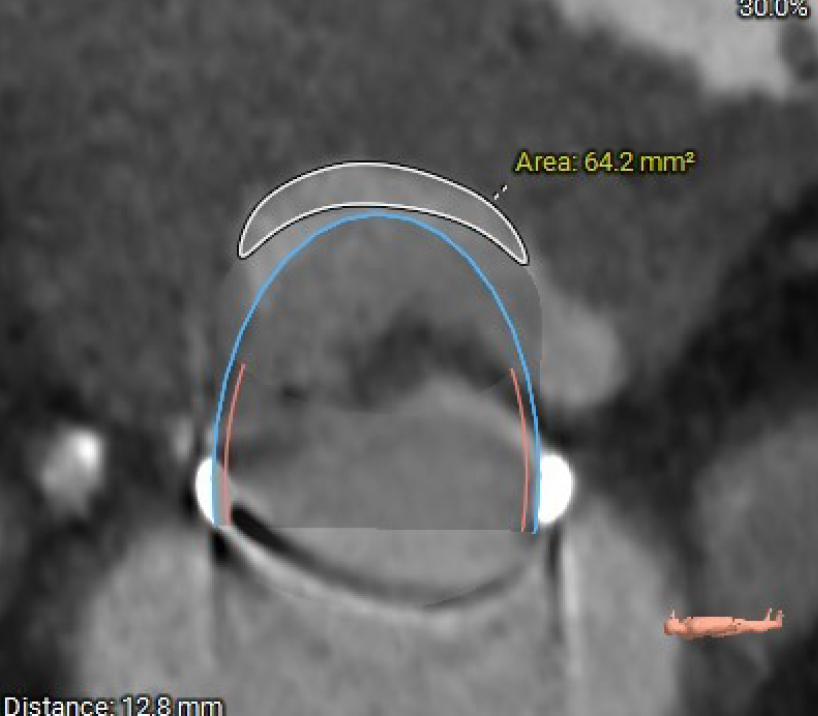
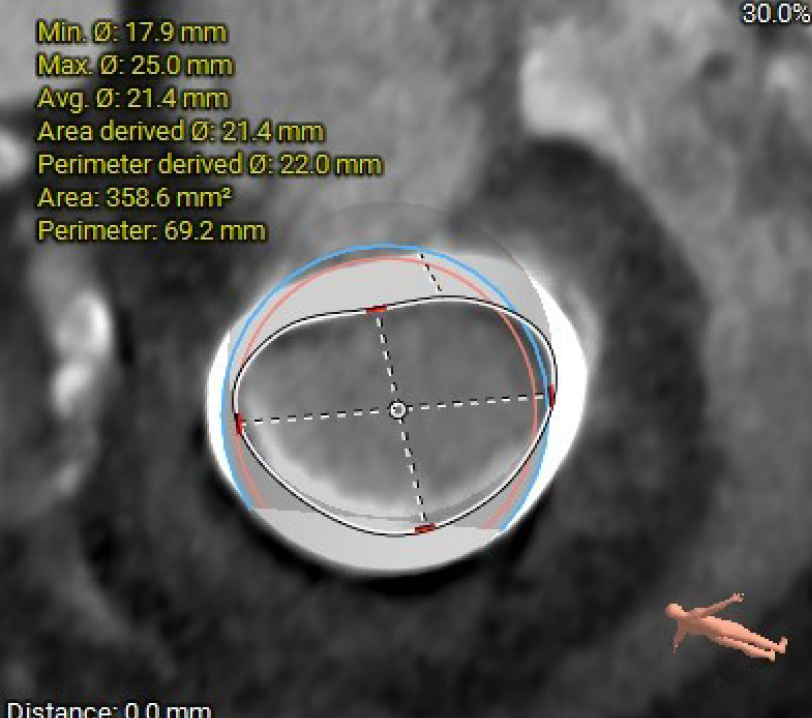
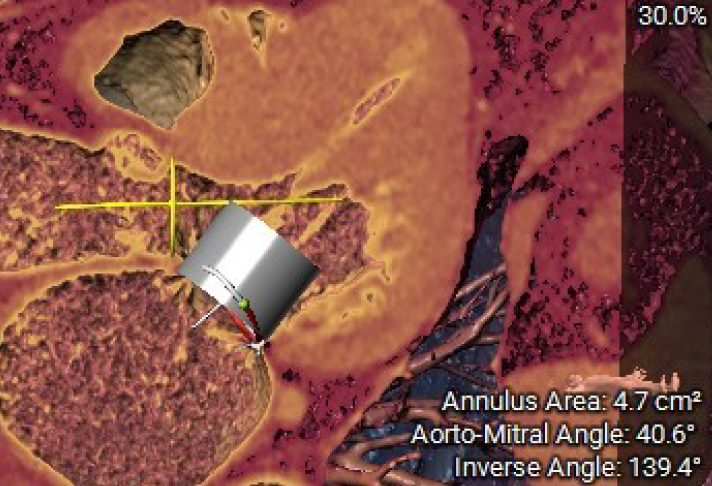
Transthoracic echocardiography revealed degenerative mitral bioprosthesis with severe regurgitation with secondary pulmonary hypertension. Multi-slice CT analysis unveiled the internal area of mitral ring is 359 mm2. The estimated neo-LVOT area is 64mm². The aorto-mitral angle measures 139 degrees.
 4C-color .mp4
4C-color .mp4
 PSL-color 2.mp4
PSL-color 2.mp4
 Mitral inflow.mp4
Mitral inflow.mp4
Relevant Catheterization Findings
Coronary angiogram revealed triple vessel disease, with severe stenosis over the middle portion of the left circumflex artery, and an ostial lesion at right coronary artery. Left ventriculography showed 3+ mitral regurgitation. Right heart catheterization showed group 2 pulmonary hypertension, pulmonary artery mean pressure 42mmHg, and pulmonary capillary wedge pressure is 26mmHg.
Interventional Management
Procedural Step
1. Before the main procedure, a Sentinel cerebral embolic protection device was implanted via the right radial artery.2. The transseptal puncture was performed under fluoroscopic and TEE guidance, and a posterior puncture was made. 3. Under the support of Agilis sheath, we use a MP/5F and Terumo guide wire to cross the mitral ring, and then up to the aorta. The Terumo wire was subsequently retrieved from the left femoral access with a JR4/7F guide catheter and a 6F Snare, forming a veno-arterial rail. Catheter rendezvous technique between MP and JR4 was performed.4. Then, the Astato XS20 wire was threaded through the catheter. Once the Astato guidewire is positioned at the tip of the anterior mitral leaflet, traction is applied to both catheters, forming a ”flying U” shape in fluoroscopy. 5. Then, the guidewire was pulled toward the base of mitral ring and electrocautery the leaflet with 40W.6. After adequate laceration, color Doppler showed splitting of regurgitant jets from the basal portion of AML, and the RT-3D TEE confirmed the laceration reached the base of the mitral annuloplasty ring.7. Septostomy was performed with a 12mm Mustang balloon for one minute.8. A 26-mm SAPIEN3 was then delivered into the ring and deployed under rapid pacing. TEE revealed no paravalvular leak, with normal transvalvular mean pressure gradients of 2 mmHg. The LVOT pressure gradient is 22mmHg.
 LAMPOON.WMV
LAMPOON.WMV
 LAMPOON 2.mp4
LAMPOON 2.mp4
 Leaflet splitting.mp4
Leaflet splitting.mp4
Case Summary
Laceration of of the Anterior Mitral Leaflet to Prevent Outflow Obstruction (LAMPOON) is a transcatheter electrosurgical technique used to split the anterior mitral valve leaflet immediately prior to transcatheter mitral valve replacement (TMVR). Our case highlights that the single-stage tip-to-base LAMPOON procedure, combined with TMVR, can be successfully performed in patients undergoing transcatheter mitral valve-in-ring (ViR) at high risk of left ventricular outflow tract obstruction (LVOTO). Incorporating the LAMPOON technique may enable us to apply TMVR to patients with a small predictive neo-LVOT area who were previously excluded based on pre-procedural evaluations.
