CASE20230516_001
Percutaneous Closure of Paravalvular Leak From a Rocking Mitral Valve in a 66-Year-Old Woman at High Surgical Risk
By Huijin Lee, Jeehoon Kang
Presenter
Huijin Lee
Authors
Huijin Lee1, Jeehoon Kang1
Affiliation
Seoul National University Hospital, Korea (Republic of)1
Other Interventions - Other Interventions
Percutaneous Closure of Paravalvular Leak From a Rocking Mitral Valve in a 66-Year-Old Woman at High Surgical Risk
Huijin Lee1, Jeehoon Kang1
Seoul National University Hospital, Korea (Republic of)1
Clinical Information
Relevant Clinical History and Physical Exam
In May 2023, a 66-year-old woman was referred for New York Heart Association functional class III fatigue and exertional dyspnea due to severe paravalvular leakage (PVL) of her prosthetic mitral valve (MV). Her medical history included scarlet fever and rheumatic heart disease, with six previous open heart surgeries (OHS) from 1986. Especially the trido-mitral valve replacement (MVR) performed to correct the mitral annular disruption in 2000.
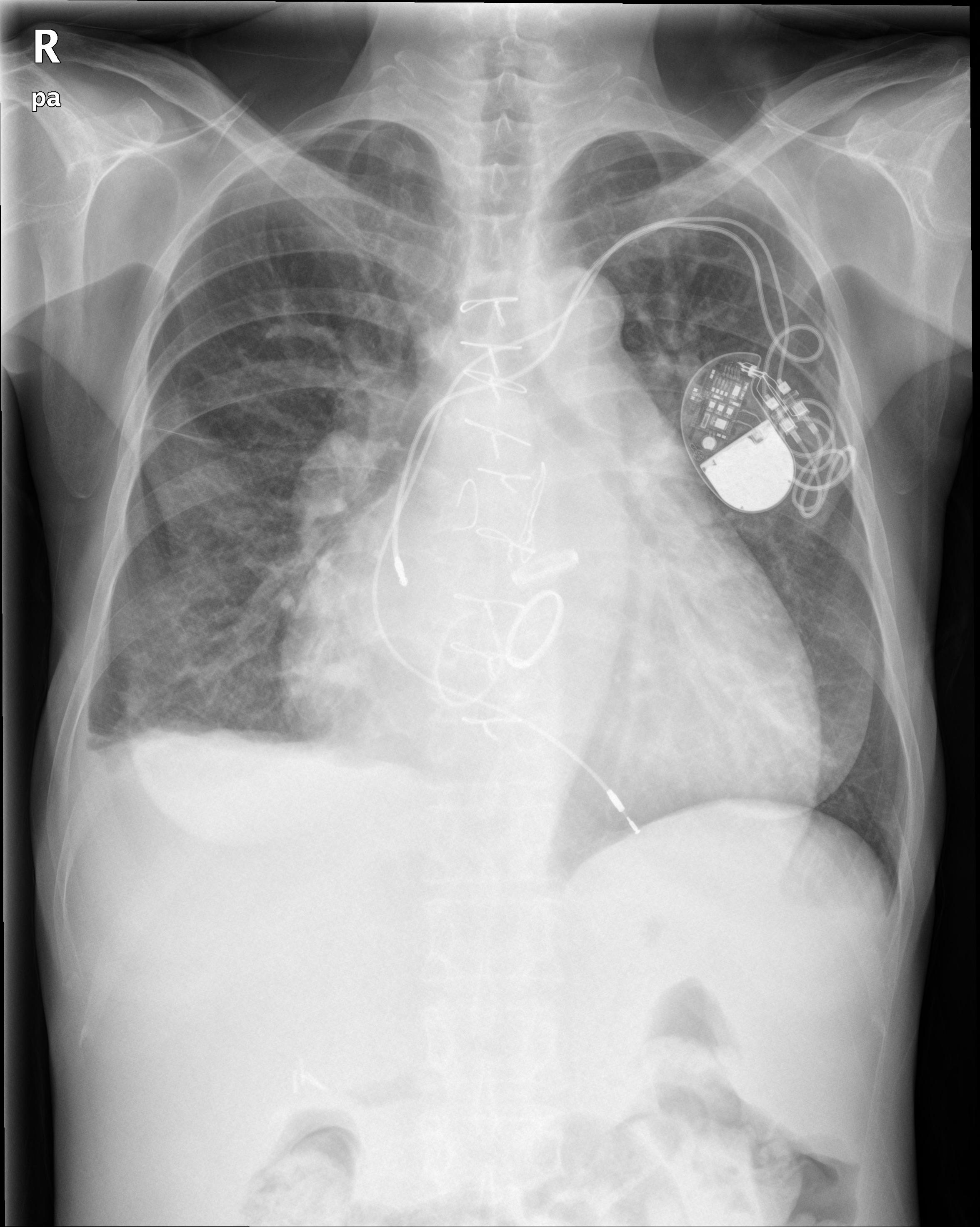
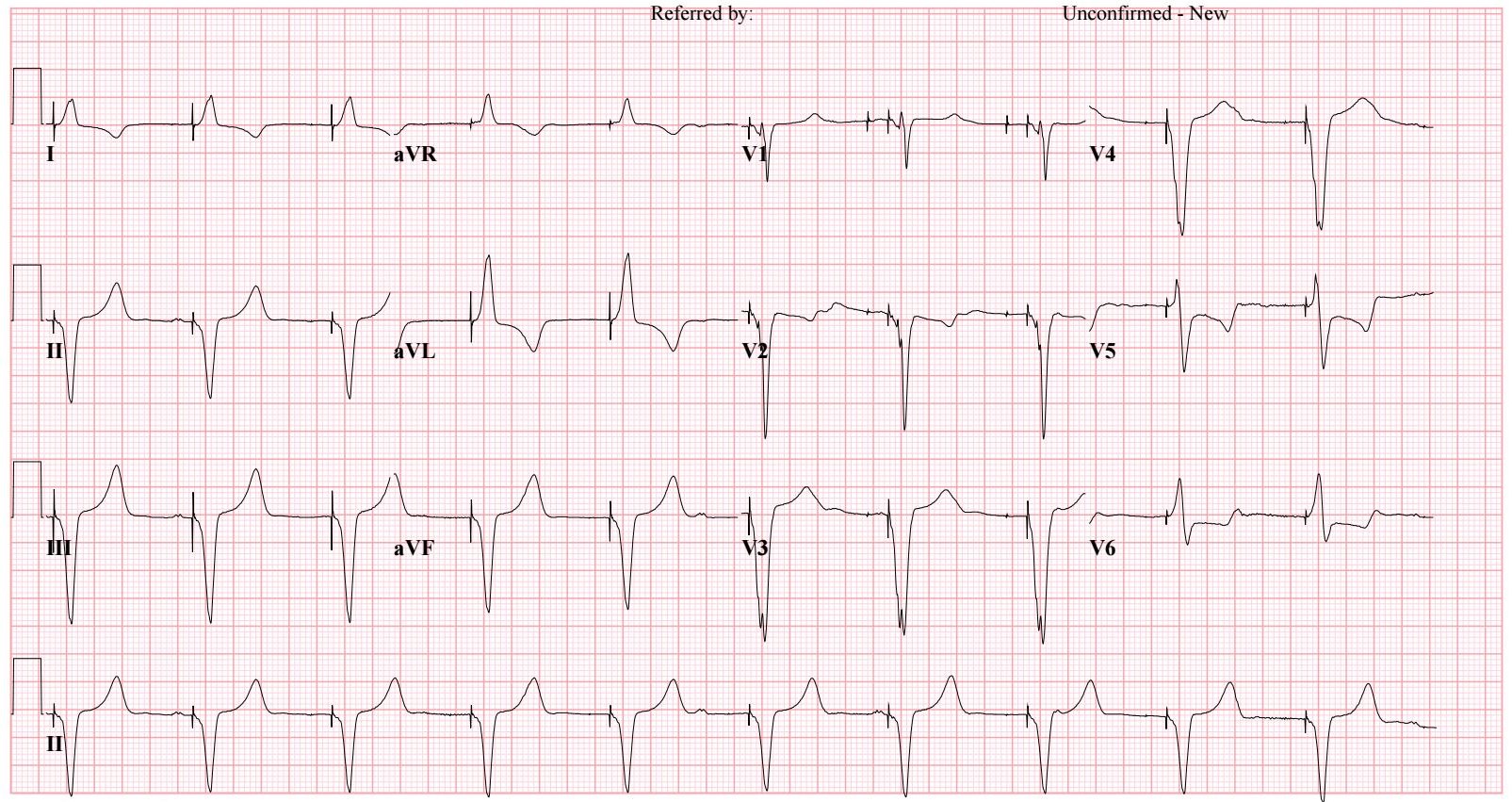
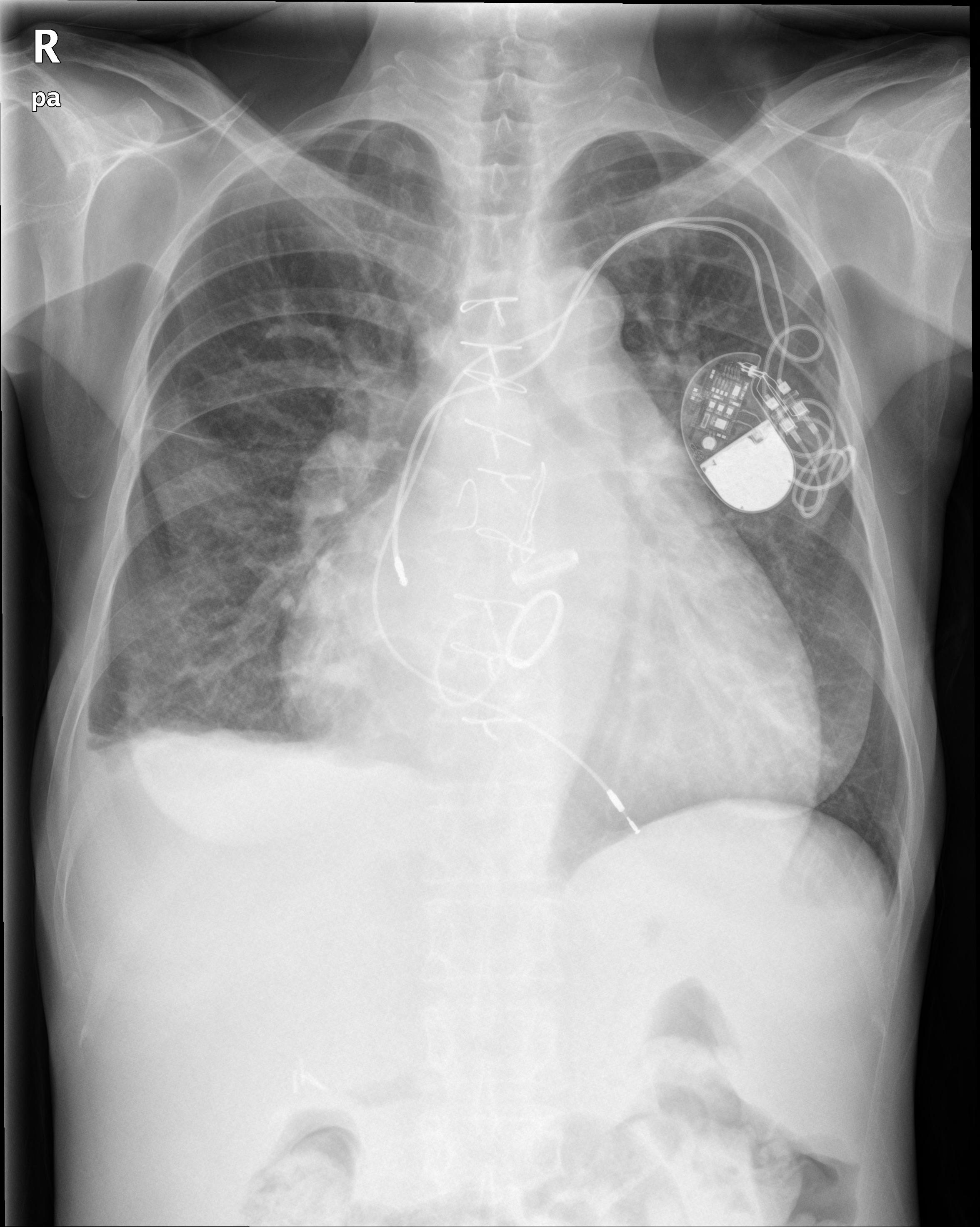
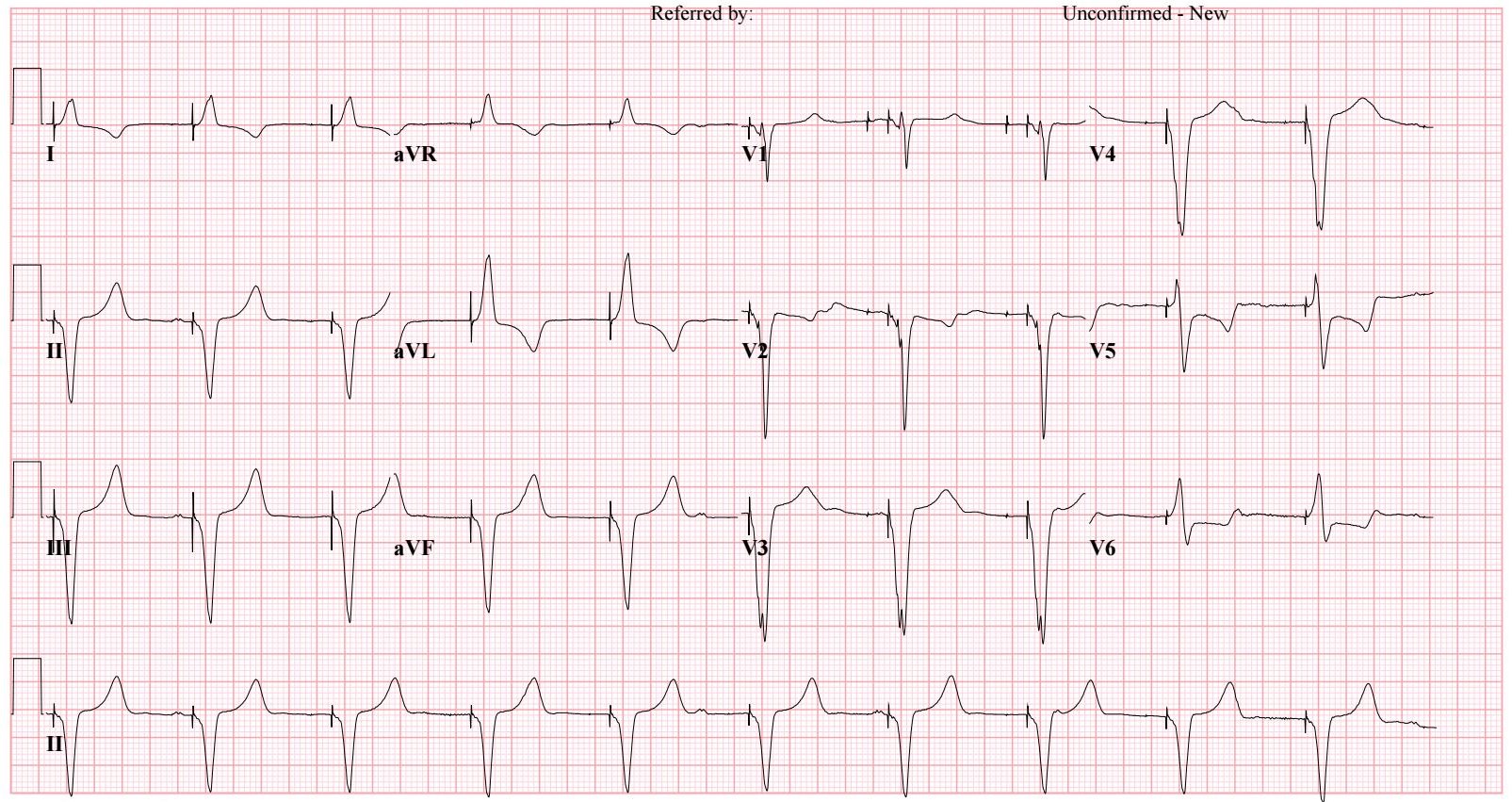
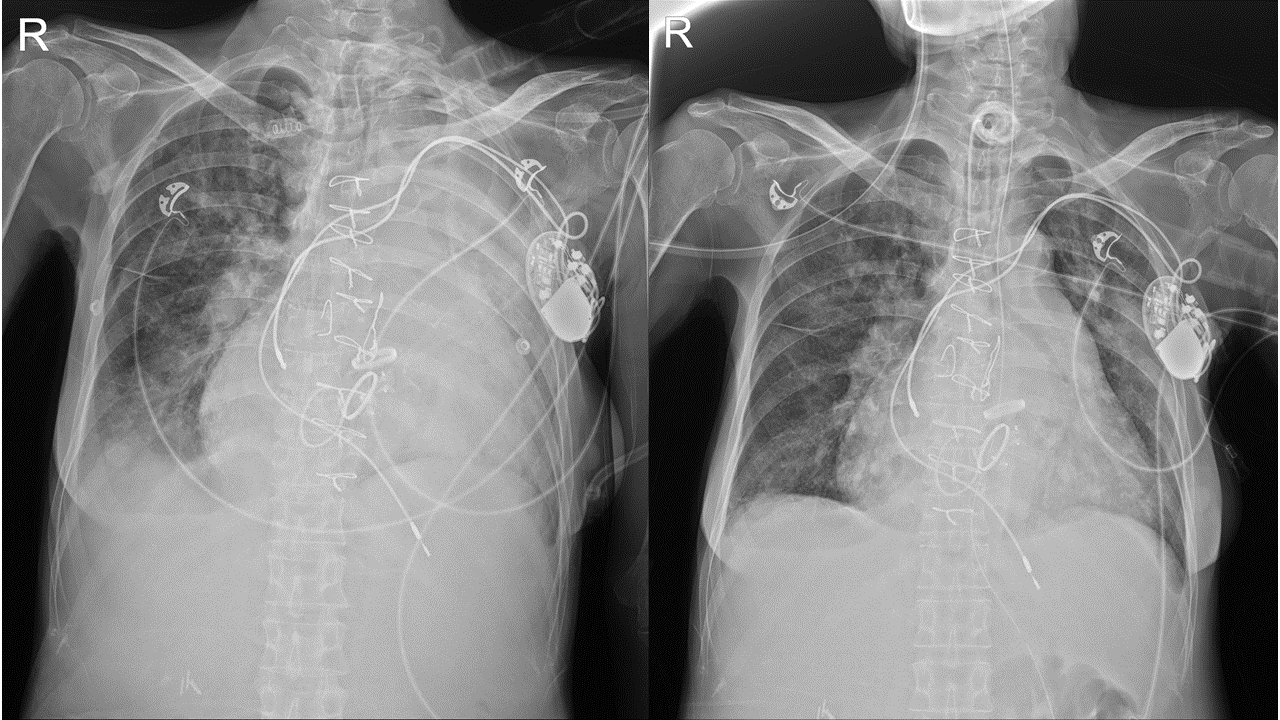
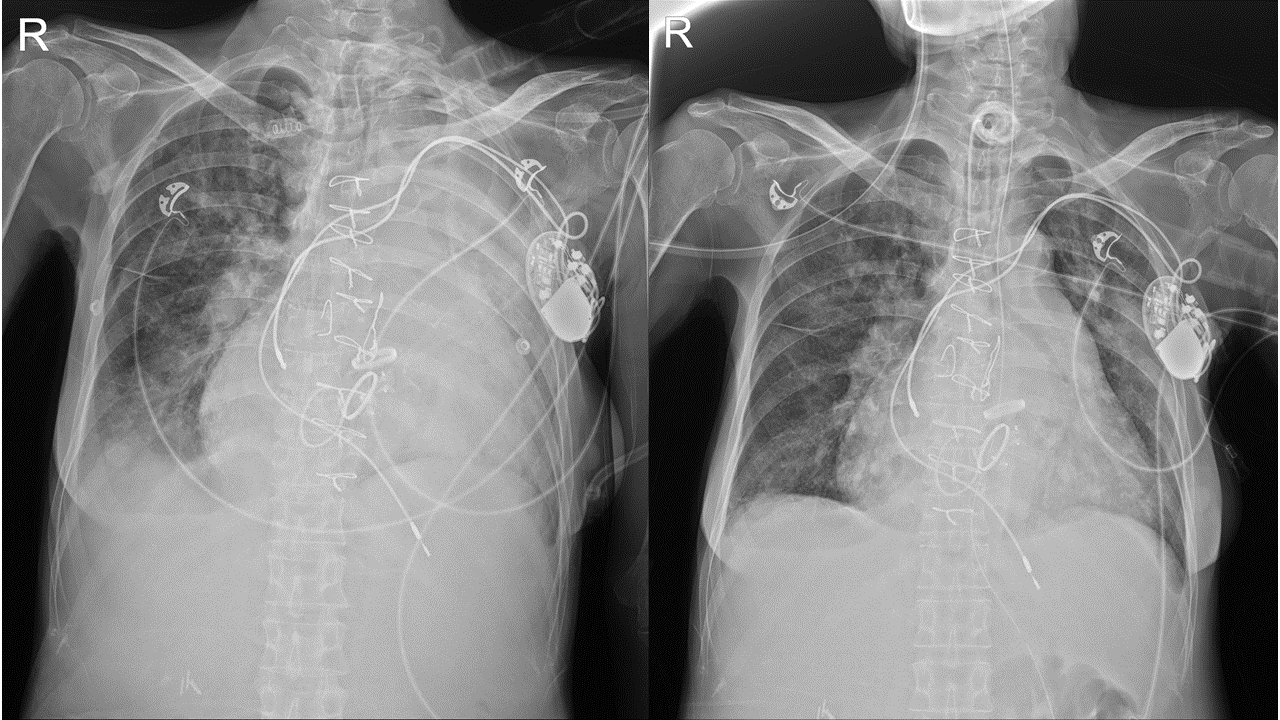
Relevant Test Results Prior to Catheterization
In echocardiography, a Dshaped left ventricular (LV) cavity with preserved LV ejection fraction and adilated right ventricular (RV) cavity with depressed RV systolic function wereconfirmed. Also, diffuse severe PVL of the prosthetic MV with rocking motionwas shown at 5-8 o’clock in Surgeon’s view.
 홍자현 TEE.wmv
홍자현 TEE.wmv
 홍자현 rocking.wmv
홍자현 rocking.wmv
Relevant Catheterization Findings
In cardiaccatheterization, group 2 pulmonary hypertension was also combined with adecreased cardiac index (C.I.) (LV end diastolic pressure 33 mmHg, mean pulmonaryartery pressure 49 mmHg, C.I. 1.89). Considering the high peri-operative (OP)risk and severe intra-thoracic adhesion, we planned percutaneous PVL closure.
Interventional Management
Procedural Step
The patient wasplaced under general anesthesia. After gaining access through the right femoralvein, we performed a transseptal puncture. Under transesophagealechocardiography (TEE) guidance, we advanced a guidewire transeptally throughthe area of the PVL into the ascending aorta. Then, successfully, we placed a12x9-mm vascular plug in the PVL area. However, right after the firstdeployment, mechanical ventilator pressure suddenly increased, and a hugeamount of fresh bloody secretion was suctioned every 5 minutes. The activatedclotting time was 239 seconds. We performed a second deployment of a 9x10mm-sizedvascular plug quickly and quit the procedure by administering Protamine 20mg.Unfortunately, TEE showed similar amounts of PVL flow at the prosthetic MV.
 홍자현 final angio.wmv
홍자현 final angio.wmv
 홍자현 postTEE.wmv
홍자현 postTEE.wmv
Case Summary
We tried toclose a severe PVL with a rocking mitral prosthesis in an elderly patient whohad a history of six previous OHS. We planned to perform the procedure becausewe judged that it is less invasive than OHS and has a lower peri-proceduralrisk. In this case, we could know that the peri-procedural risk is not lowerthan the peri-OP risk. Underestimating the peri-procedural riskdue to the less-invasiveness of the procedure should be thought of as anotherrisk factor of the procedure.
