Upfront Protection Needed for 'Rare But Real' Risk of TAVR-related Coronary Artery Occlusion
[AP VALVES & SH 2021] Expert highlights when and how to protect at-risk arteries for TAVR patients
Interventional teams need to pan out and choreograph the identification, prevention, and procedural techniques for coronary artery occlusion (CAO) that can occur duringtranscatheter aortic valve replacement (TAVR), an expert said recently.
Employing strategies before and during the procedure, such as a pre-procedural CT or primary bail-out procedural techniques like "chimney" (snorkel) stenting and BASILICA, can mitigate the risk of TAVR-related CAO.
 Lars Sondergaard, MD (Copenhagen University Hospital Rigshospitalet, Copenhagen, Denmark) emphasized these points during an online 'Live Case & Lecture 2: TAVR - Coronary Access' lecture at the 10th AP Valves & Structural Heart Virtual (AP VALVES & SH 2021) conference on Aug. 5.
Lars Sondergaard, MD (Copenhagen University Hospital Rigshospitalet, Copenhagen, Denmark) emphasized these points during an online 'Live Case & Lecture 2: TAVR - Coronary Access' lecture at the 10th AP Valves & Structural Heart Virtual (AP VALVES & SH 2021) conference on Aug. 5.
"The lesson here is this," Sondergaard said. "If you are concerned about coronary artery occlusion during the procedure, then protect it upfront."
CAO is a rare but highly fatal complication that may occur during TAVR through either a direct obstruction of coronary flow (i.e., displaced native leaflet tissue of the valve flows towards coronary ostium) or an indirect reduction of coronary flow (i.e., displaced leaflet tissue contacts the sinotubular junction and seals off coronary sinuses).
Such occlusions of the coronary artery rarely occur, accounting for less than 1% of TAVR cases, but they carry a high risk of mortality of about 40-50%1.
"Coronary artery occlusion during TAVR is a rare but often fatal complication; it is important to identify patients at risk, and we can do this by assessing certain characteristics," said Sondergaard. "Most often, the complication occurs in patients undergoing valve-in-valve (ViV) procedures due to failing or degenerative surgical bioprosthetic valves. So screening with pre-procedural CT for certain high-risk anatomical features can lower risk."
For procedural techniques, he said: "Chimney stenting is relatively simple and safe but has re-accessing and stent failure concerns, while the BASILICA that is taking off in Europe and the U.S. is also an option, but it's more technically challenging and carries a risk of failure."
'ViV procedures, certain coronary features raise TAVR-related CAO risk'
TAVR-related CAO is a bigger problem in native aortic valves with distinct coronary height coronary sinus, and/or aortic root size, Sondergaard said, as well as for patients undergoing ViV procedures for degenerated bioprosthetic aortic valves.
For patients with native aortic valves, characteristics that heighten CAO risk include low coronary take-off, shallow sinus of the Valsalva, low sinotubular junction, and long, calcified cusps; these elements call for pre-procedural coronary protection.
Opposing these characteristics are the "low-risk" elements such as high coronary take-off, wide Valsalva sinus, high sinotubular junction, and short, non-calcified cusps.2
For TAVR in degenerated surgical bioprostheses, Sondergaard also flagged low coronary take-off, shallow sinus of Valsalva, or low sinotubular junction as higher-risk.
Surgical bioprostheses with externally mounted leaflets or short valve-to-coronary (VTC) distance (< 4 mm) require extra caution, he added.
Insights from the VIVID registry3 that examined the CAO risk according to the type of surgical bioprosthesis showed that the risk was significantly higher in patients stented with externally mounted leaflets than those stented with internally mounted leaflets (6.4% vs. 0.7%, p<0.001).
In light of problems of surgical valves with externally mounted leaflets, Sondergaard explained that the Mitroflow (Sorin Group) stented bioprosthesis; Trifecta (Abbott) stented bioprostheses; and the Freedom Solo (Sorin Group) stentless bioprosthesis with "leaflets sutured outside the stent" pose a greater risk than the Mosaic (Medtronic) bioprosthesis.
"Coronary artery obstruction is a rare side effect, but it's a real risk for valve-in-valve procedures, especially with externally mounted leaflets," he said. "Pre-procedural CT can help identify patients at risk, so the at-risk artery should be protected upfront if occlusion during TAVR is a concern."
Chimney stenting for compromised coronary blood flow during TAVR
Chimney stenting, originally used as a repair procedure for endovascular aneurysms, is now one of the primary bail-out techniques used to restore occluded blood flow during TAVR.
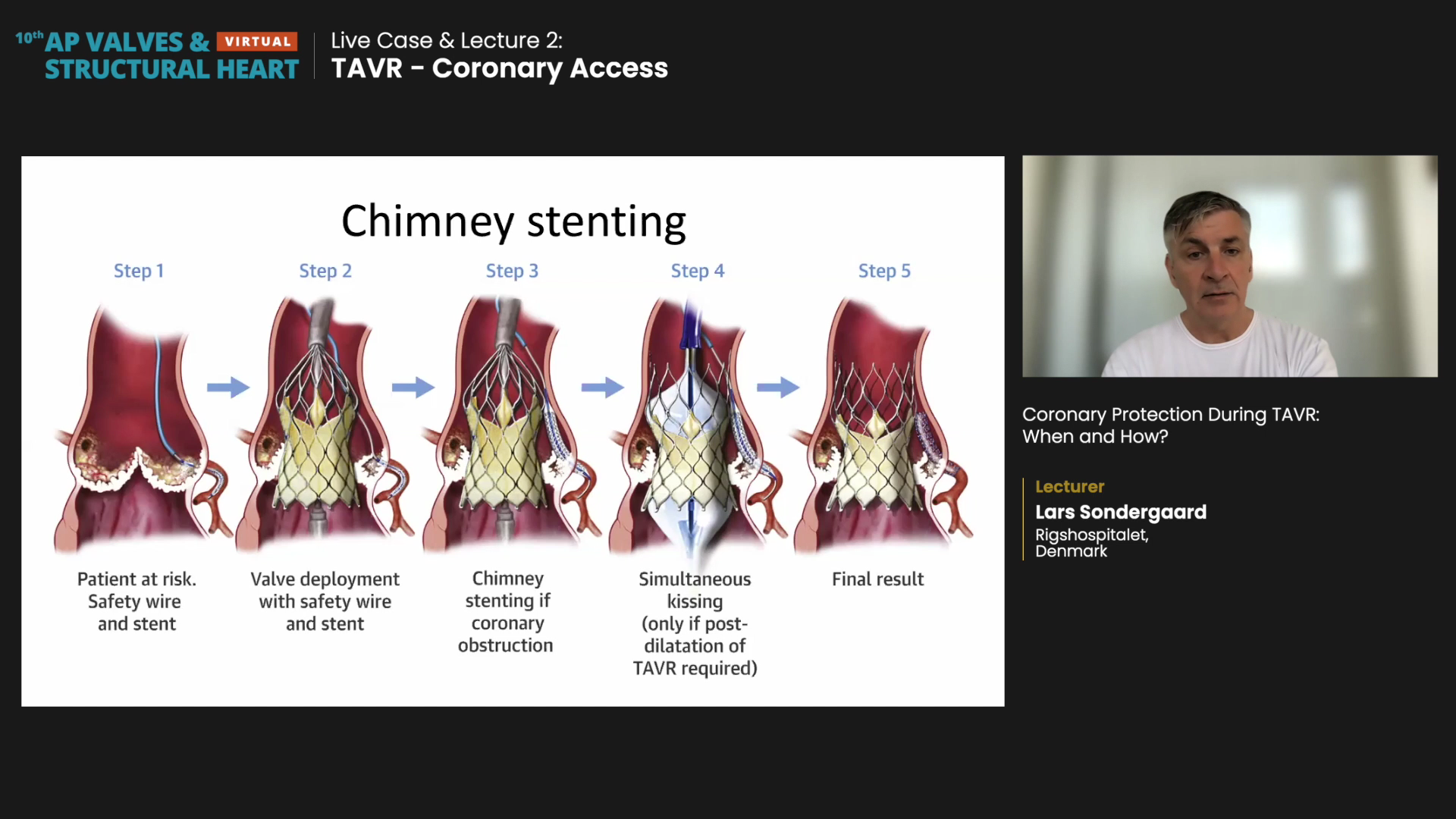
Real-world CHIMNEY registry data4 on 12,800 TAVR procedures across 16 centers in North America, Europe, and the Middle East showed that chimney stenting was performed on only 60 patients, indicating underutilization. Of the 60 cases, 70% were for ViV and 30% for native aortic annulus.
30-day clinical outcomes showed patients with established CAO (eCAO) had worse results than those with impending CAO (iCAO).
Myocardial infarction (MI) did not occur in any iCAO patients but in half of eCAO patients. eCAO patients also had more cardiogenic shock as well as increased need for mechanical circulatory support, extracorporeal membrane oxygenation, and cardiopulmonary resuscitation or defibrillation.
Upfront coronary protection was performed on 73% (44/60 patients) and was as a sole independent risk factor for the composite endpoint of death, cardiogenic shock, or MI. Not protecting the at-risk artery elevated outcome risks 7-fold according to multivariate analysis (OR 7.39, 95% CI 1.95-27.93, p<0.01).
The rate of stent failure after chimney stenting was 3.5% after a median follow-up of 612 days. The two patients reported stent failure on day 157 (in-stent restenosis) and day 374 (possible late-stent thrombosis).
"Although complication rate is low, chimney stenting has a much higher risk of procedural death, stroke, and vascular complications," Sondergaard said. "Another potential area for concern would be the difficulty of accessing the coronaries down the road."
Novel BASILICA shows good outcomes with few complications
Although more technically challenging, BASILICA is a safe and effective way to bail out CAO during TAVR and decrease re-accessing risk since it avoids placing a coronary stent in the aorta.
BASILICA is an acronym for bioprosthetic aortic scallop intentional laceration to prevent Iatrogenic coronary artery obstruction.
The novel transcatheter electrosurgical cusp-lacerating technique, originally used only compassionately, proved safety and effectiveness in a prospective, multicenter, single-arm safety and feasibility BASILICA trial that reported 30-day outcomes in 20195 and recent 1-year results on May 18.6
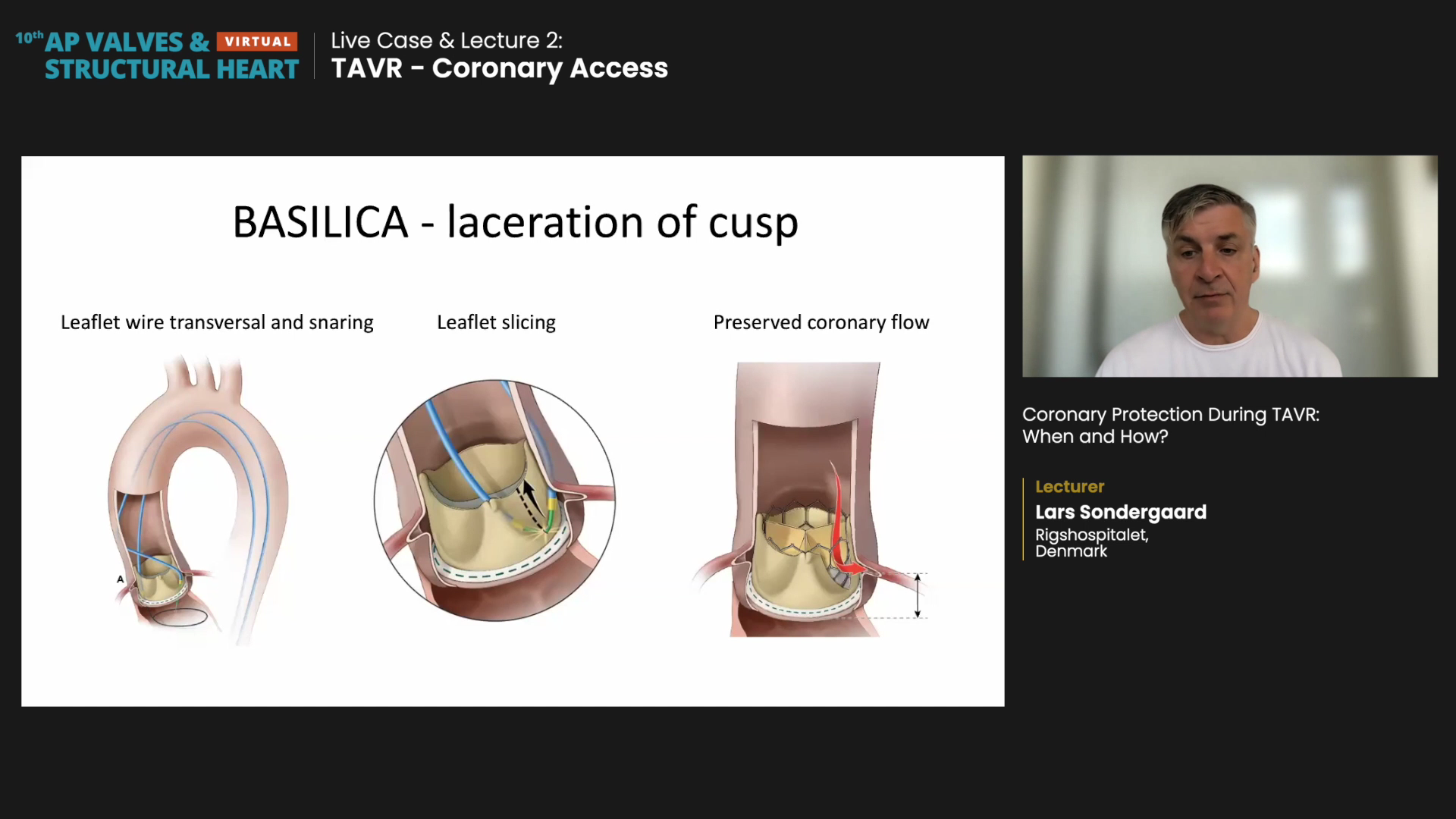
During the procedure, the operator inserts a leaflet wire catheter in front of the coronary arteries (i.e., transversing the left/right aortic leaflet) and then snares the wire, pulling it back with leaflet slicing to lacerate the cusp from the base so that coronary artery flow is possible after valve implantation.
The study included 30 patients with severe native aortic valve (43%) or bioprosthetic aortic valve disease (57%) at high- or extreme-risk for surgery and increased CAO risk. The primary endpoint was death, stroke, and MI at 1-year.
At 30-days, BASILICA was successful in 93.3% (28 patients) but reported cases of 3 strokes (10%), including 1 disabling stroke (3.3%), 1 death (3.3%), and 1 periprocedural MI (3.3%).
At 1-year follow-up, investigators reported 2 deaths (10% 1-year mortality) but no additional cases of stroke or MI.
Further analysis of 1-year outcomes showed certain anatomical features strongly indicated favorable results. Anatomical strengths for the BASILICA procedure included:
- Typical calcium patterns that spare the leaflet nadir
- Commissures aligned with native commissures
- "Ergonomic" femoral access for BASILICA catheters
- Single-leaflet BASILICA
- Risk from sinus sequestration
Characteristics that indicate a poor match for BASILICA included confluent calcium at the leaflet nadir, bulky calcium mass on the leaflet, and bioprosthetic valve post in front of the coronary artery ostium.
Double-leaflet BASILICA was not recommended for cases of nonfemoral access (femoral artery or transcaval) as well as for relatively inexperienced operators in their first cases (less than 3 procedures).
For ViVs with bicuspid valves, balloon aortic valvuloplasty for coronary flow assessment, simultaneously performed with an aortic root injection can help confirm unaffected coronary flow and clear the patient for TAVR. Other precautions, such as having a surgeon in the operating room and priming the heart-lung machine, can help mitigate TAVR outcomes, Sondergaard said.
- https://www.sciencedirect.com/science/article/pii/S1936879820302673?via%3Dihub
- https://www.jacc.org/doi/full/10.1016/j.jcin.2020.01.227
- https://academic.oup.com/eurheartj/article/39/8/687/4082639
- https://www.jacc.org/doi/full/10.1016/j.jcin.2020.01.227
- https://www.acc.org/latest-in-cardiology/articles/2019/08/18/24/42/feature-cutting-edge-structural-interventions-the-basilica-procedure
- https://www.ahajournals.org/doi/abs/10.1161/CIRCINTERVENTIONS.120.010238
Edited by

Duk-Woo Park, MD
Asan Medical Center, Korea (Republic of)
Written by


